Sacroiliac Joint Stabilization Techniques
Fixation/traditional fusion with cannulated screws
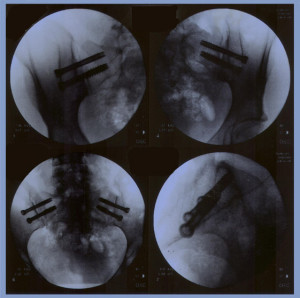 After the patients SI joint is manually corrected into proper position by a skilled physical therapist, the patient is placed prone on a radiolucent table to allow the use of an image intensifier. The aim of the operation is to insert two cannulated screws from the ilium into the sacrum. Monitoring proper placement is achived with the image intensifier by a trained technician who alerts the surgeon when close to a nerve root to avoid injury to the sacral nerve roots.
After the patients SI joint is manually corrected into proper position by a skilled physical therapist, the patient is placed prone on a radiolucent table to allow the use of an image intensifier. The aim of the operation is to insert two cannulated screws from the ilium into the sacrum. Monitoring proper placement is achived with the image intensifier by a trained technician who alerts the surgeon when close to a nerve root to avoid injury to the sacral nerve roots.
The patient is positioned so that an anterior view can be taking in a 40 cephalad neutral and 40 caudal position. A point three finger breadths lateral and at a 45 angle distal to the posterior spine is used for insertion of an 18-gauge spinal needle aiming the needle at about a 45 angle towards the PSIS. Image intensification confirms that the needle is appropriately placed in AP and lateral views. Sometimes it takes serveral repositionings of the needle to get an appropriate position.
Once the position is determined, two Steinmann pins are inserted across the joint under EMG monitoring and under image intensification guidance. Once it is determined that the Steinmann pins are in an appropriate position, incisions are made, the depth of penetration measured and appropriate-sized 6.5 cannulated screws placed across the joint. Once again, the pins should be tested to make sure there is no evidence of any nerve root irritation and, there being none, the pins are removed. The incisions are irrigated, and closed with the suture of choice. If the patient’s problem is purely extra-articular, that completes the operation.
If the patient has joint problems, a posterior skin incision can be made parallel and slightly medial to the posterior sacroiliac spine extending cephalad and parallel to the iliac crest. The lumbodorsal fascia, as it inserts onto the inner table of the ilium is identified and stripped from its attachment, exposing the inner table of the ilium. Using osteotome mallets, gouges and curettes, a bone graft is harvested from the inner table. This not only allows for better visualization of the ligaments and joint, but also gives bone graft for future grafting.
The ligamentous portion is noted in the depths of the wound and more distally, the cartilaginous portion of the joint as it tucks under the long dorsal ligament. Care is taken to avoid entering the sciatic notch. Using gouges, curettes, and tissue rongeurs, the ligamentous and cartilaginous portion of the joint are removed. The defect thus created can be prepared by decorticating the inner table of the ilium and the outer portion of the sacrum. This can be done with a burr, if desired.
Once the bone is decorticated, the bone graft is inserted. Supplemental allograft can also be used. The lumbodorsal fascia is reapproximated and the subcutaneous and skin closed.
.